Percutanoues Laser Disc Decompression
Safe and effective minimally-invasive non-surgical technique invented by dr. Daniel Choy in 1986.
History
In mid-February 1986, dr. Peter Ascher and dr. Daniel Choy performed the first percutaneous laser disc decompression (PLDD) procedure at the Neurosurgical Department, University of Graz, Graz, Austria. It was planned to deliver 1000 J of energy with an Nd:YAG laser 1064nm for a herniated L4-L5 disc causing sciatica. At 600 J the procedure was terminated because the pain was gone.
Treatment Principle
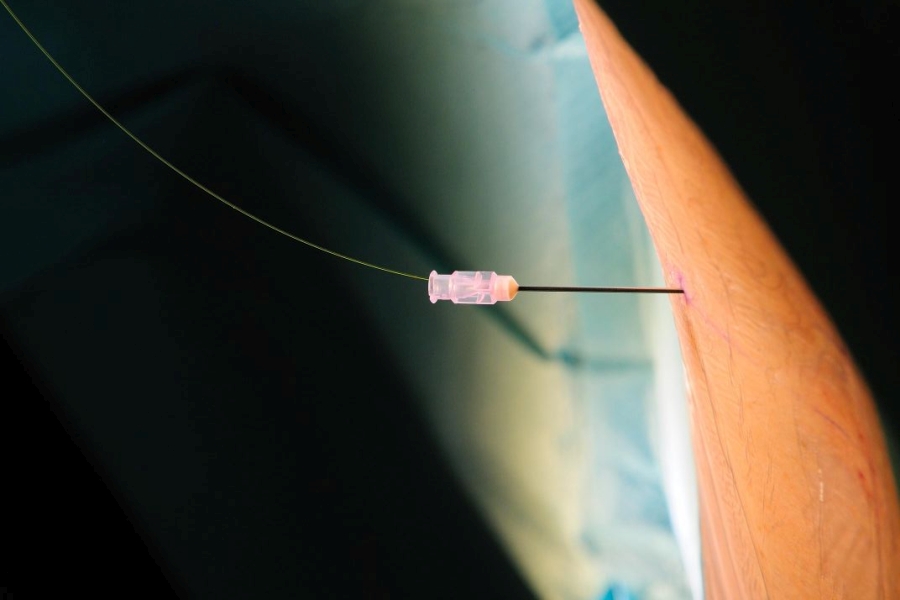
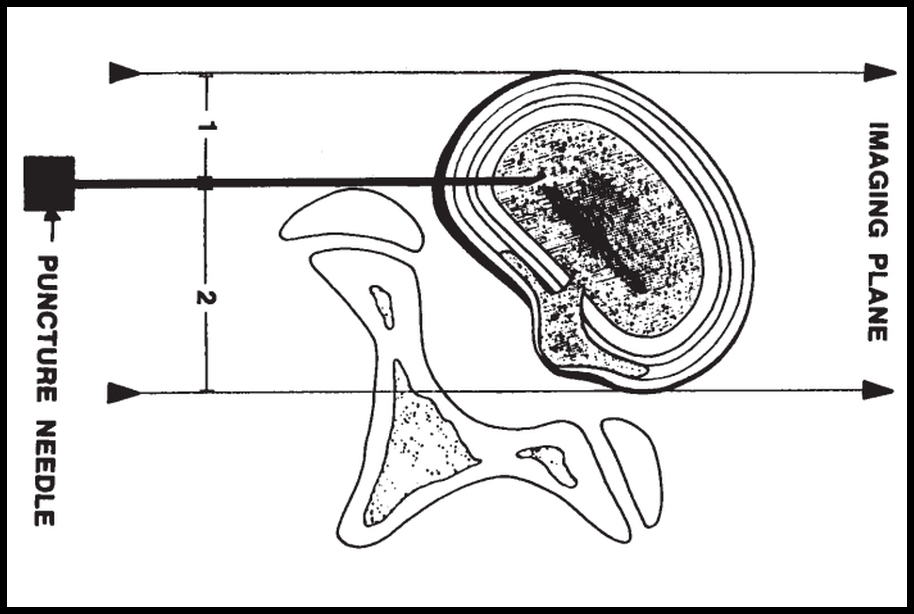
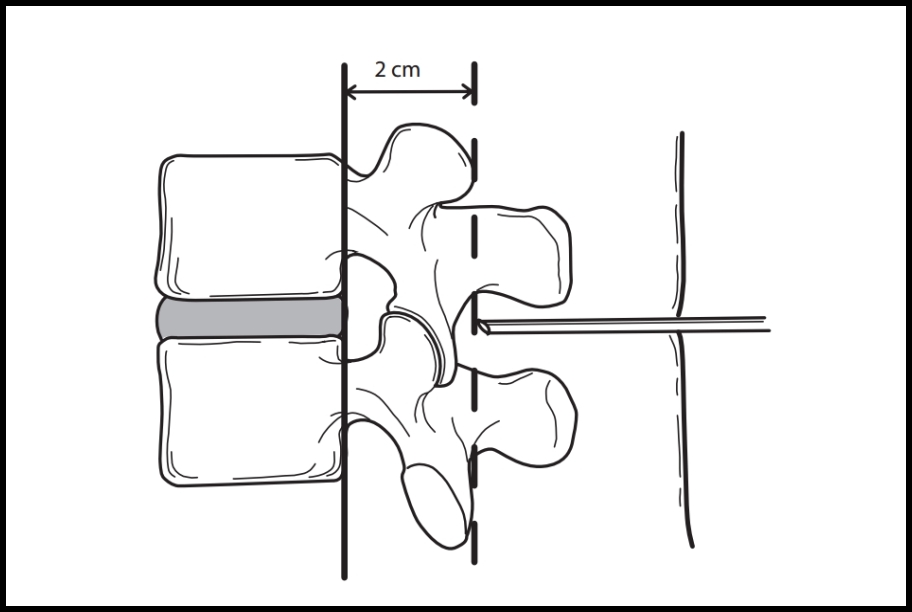
The treatment principle of PLDD is based on the concept of the intervertebral disc being a closed hydraulic system. This system consists of the nucleus pulposus, containing a large amount of water, surrounded by the inelastic annulus fibrosus. An increase in water content of the nucleus pulposus leads to a disproportional increase of intradiscal pressure. A reduction of intradiscal pressure causes the herniated disc material to recede toward the center of the disc, thus leading to reduction of nerve root compression and relief of radicular pain (leg pain and/or back pain). In the PLDD, this mechanism is due to the application of laser energy evaporating a small amount of water in the nucleus pulposus. Laser energy is delivered by a laser fiber through a tiny needle placed into the nucleus pulposus. The needle is placed into the intervertebral disc under local anesthesia. Apart from evaporation of water, the increase in temperature also causes protein denaturation and subsequent renaturation (biochemical effect of laser energy into the nucleus pulposus). This causes a structural change of the nucleus pulposus, limiting its capability to attract water and therefore leading to a permanent reduction of intradiskal pressure.
Procedure technique
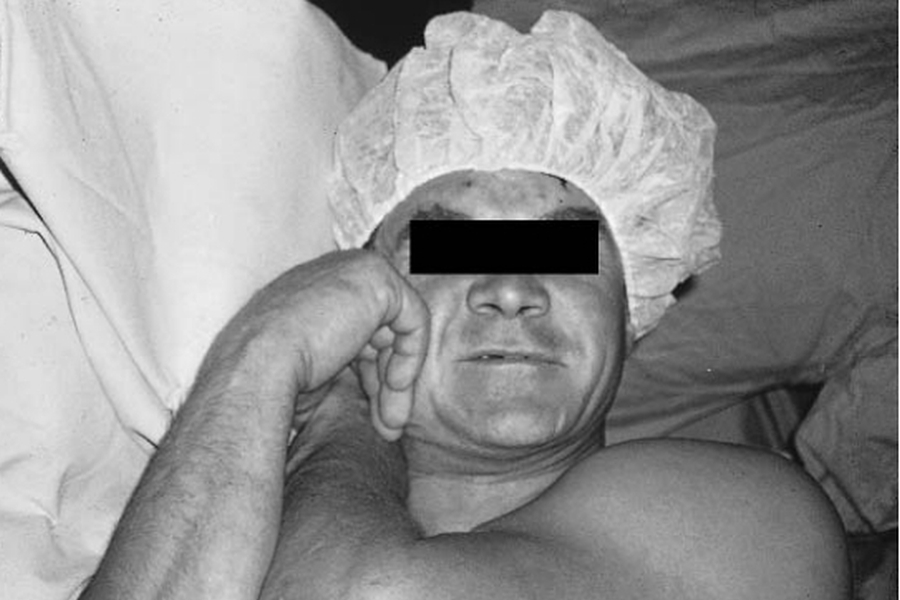
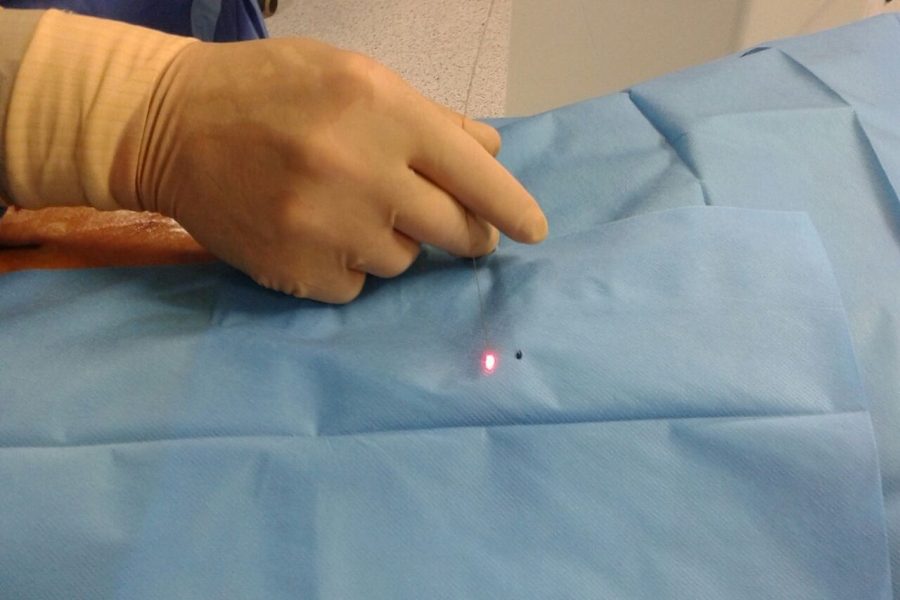
The procedure is conducted under local anesthesia of the skin and underlying muscles, so there are no risks associated with general anesthesia and no risk of nerve root injury because of patients contact feedback. After assessment of the correct disc level by using intraoperative fluoroscopy, a needle is inserted into the center of the disc. When the needle is in place, its correct position is verified by using biplanar fluoroscopy. A laser fiber is inserted through the needle into the center of the nucleus pulposus and its tip comes out of about 5-8 mm from the needle tip. Laser energy is then delivered into the nucleus pulposus to vaporize its content and reduce intradiscal pressure.
There is a considerable degree of variation in the way PLDD is performed around the world. Differences can be found in the choice of laser type and laser parameters used, and imaging techniques used during the procedure.
Our chief professor, dr. Gian Paolo Tassi, applies and teaches this technique to other students/fellows according to the prof. Daniel S. J. Choy's technique (Columbia University of New York, the inventor of PLDD in 1986 and the preceptor on the PLDD of dr. Gian Paolo Tassi at the Laser Spine Center, New York).
Indications / selection criteria
PLDD procedure can be performed anywhere on the spine (cervical, thoracic, lumbar - except T1-T9 discs). Indications/clinical findings that could be suitable for PLDD procedure:
- Herniated disc (bulged, protruded and even extruded discs but with a good "bridge" between the extruded part and the parent disc)
- Spinal stenosis (where herniated disc is almost or more than 50% of the contributing factor)
- Discogenic pain (due to slipped disc or internal disc disruption)
- Sciatica (due to slipped disc)
Treatment Outcome: Success Rates and Complications
Since 1986 PLDD has spread all over the world, with procedures being performed throughout the entire spine, with exception of T1-T9 disc treatment due to very high risk of pneumotorax. The success rate has ranged from 70% to 89%, and the complication rate, chiefly discitis, from 0.1% to 1.0%. When successful, the return to normal work is in from 2-4 weeks, depending on the patient's job. The long-term follow-up of 23 years has yielded a recurrence rate of 5%.
Experience of professor dr. Gian Paolo Tassi with 3869 PLDD procedures (September 2016.) shows 83,8% of possitive results, 4% of reccurence cases and only 0,1% of discitis related complications.
Benefits for your patients:
- Minimally-invasive
- Maximally-effective
- No cutting
- No scarring
- No anesthesia
- No or very short hospital stay
- Quick recovery
- Less cost than traditional and endoscopic surgery
dr. Gian Paolo Tassi - teacher

Quick facts:
- Trained by dr. Daniel Choy
- Worldwide experience since 2002.
- Greatest experience in world
- 83,8% success rate
- 4% recurrence rate
- 0,1% discitis (4 patients)
- No serious complications